We started our KPI series with A/R Days, the next one is Denial Rate. There are a couple of them, the one I’ll cover here is Remit Denial Rate.
Why is it important?
Denial prevention and appeals have been and continue to be one of the most resource draining activities of Revenue Cycle Management (RCM). No one wants to do it, one may even think they shouldn’t have to do it (those evil payers). But denial prevention and appeals is a piece of RCM, and when done right, will recover cash that will contribute directly to overall financial health and funds the care your patients need.
What’s the calculation?
One will need to categorize the CARC and RARC codes between “actionable/preventable” from those that are not. For example, CARC code 29 “The time limit for filing has expired.” is preventable, where as CARC code 45 “Charge exceeds fee schedule/maximum allowable or contracted/legislated fee arrangement” is expected and not actionable.
What is the benchmark?
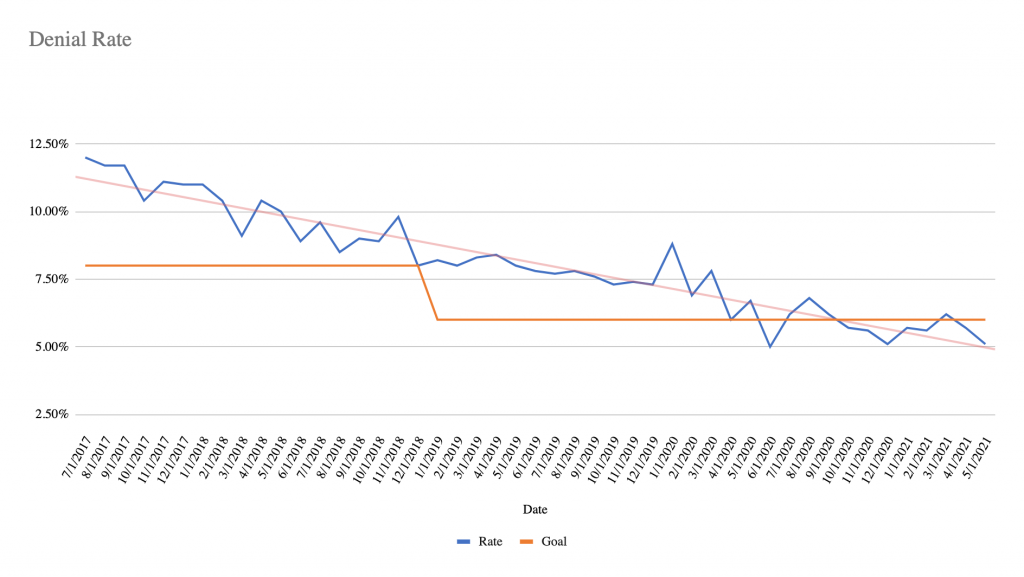
7% is average and 5% is best practice, pre-pandemic. While the pandemic rages on and staffing shortages prevail, averages are around 10% with some areas seeing spikes as high as 14%.
If you are just starting out tracking denial rates, your denial rate might be rather high. And in some areas like “No authorization” or “Not medically necessary” where you are relying on a clinical area for prevention, these may seem impossible to address, but essential for best practice denial management.
How often should I update?
For operational support, denial rates should be measured for weekly trending based on the most recent week’s remittances. You will want to roll those up for a monthly report for your health system’s leadership team.
Where do I get my data?
Your most recent week’s remittances.
I strongly recommend converting paper remittances to electronic. You could have some significant cash hidden in that paper that won’t come to light until you aggregate the data in an understandable and standard format.
What does it look like?
What else?
- Medicare Return to Provider rate (RTP)
- Denial rate by payer
- Denial recovery Rate
- Clean claim submission rate
These will become active links when the articles are available.

